

For the Beijing Chaoyang Hospital, IRB approval was provided by Beijing Chaoyang Hospital IRB/EC, Beijing, China. For the Peking Union Medical College Hospital, IRB approval was provided by the Peking Union Medical College Hospital IRB/EC, Beijing, China. For the Asker and Baerum Hospital, IRB approval was provided by the Regional Committee for Medical Research Ethics for South-East Norway (B), Oslo, Norway. For the Vejle Hospital, IRB approval was provided by The Ethical Committee of Science for the Syddanmark Region, Vejle, Denmark.

For the University Hospitals Leuven, IRB approval was provided by UZ Gasthuisberg Central IRB/EC, Leuven, Belgium. The study was conducted in accordance with principles of Good Clinical Practice and was approved by the appropriate Institutional Review Board (IRB)/Independent Ethics Committee at each study site. The study was conducted at six sites in China and four sites in Europe (two sites in Denmark and one site each in Belgium and Norway). This was a randomized, parallel-group, multicenter, safety-assessor-blinded study ( NCT00825812 protocol P05768), conducted from February to September, 2010. Key secondary objectives were to show faster recovery from rocuronium-induced NMB with sugammadex vs neostigmine in Caucasian subjects and to demonstrate equivalence in recovery times between Chinese and Caucasian subjects.
#ATROPINE ANTIDOTE NEOSTIGMINE PLUS#
The primary objective of the present study was to investigate efficacy and safety of sugammadex 2 mg/kg compared with neostigmine 50 μg/kg plus atropine 10–20 μg/kg for reversal of moderate rocuronium-induced NMB in Chinese and Caucasian subjects. Sugammadex is marketed for reversal of rocuronium- and vecuronium-induced NMB in over 40 countries worldwide.ĭata on the efficacy and safety of sugammadex in Chinese subjects are required. Furthermore, sugammadex is equally effective for reversal of rocuronium-induced NMB under both propofol and sevoflurane maintenance anesthesia.
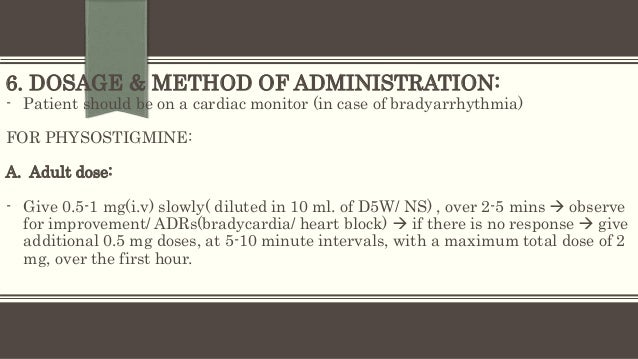
The selective relaxant-binding agent sugammadex (Bridion®, MSD, Oss, The Netherlands) has been shown to rapidly and completely reverse the effects of the NMB agents rocuronium and vecuronium. However, these agents may provide slow and unpredictable recovery, and are associated with several unwanted side-effects, both alone and in combination with anticholinergic agents. Acetylcholinesterase inhibitors such as neostigmine are commonly administered to reverse NMB at the end of surgery and to reduce the risk of residual paralysis and associated adverse respiratory events. Neuromuscular blockade (NMB) is often used during surgery to facilitate tracheal intubation and to improve surgical conditions.
#ATROPINE ANTIDOTE NEOSTIGMINE TRIAL#
Trial registrationĬ Identifier: NCT00825812. Conclusionīoth Chinese and Caucasian subjects recovered from NMB significantly faster after sugammadex 2 mg/kg vs neostigmine 50 μg/kg, with a ~5.7 times ( p < 0.0001) faster recovery with sugammadex vs neostigmine in Chinese subjects. There was no residual NMB or recurrence of NMB. Sugammadex 2 mg/kg was generally well tolerated, with no serious adverse events reported. Corresponding times for Caucasian subjects were 1.4 (1.3–1.5) min and 6.7 (5.5–8.0) min, respectively. Geometric mean (95% CI) time to recovery to TOF ratio 0.9 was 1.6 (1.5–1.7) min with sugammadex vs 9.1 (8.0–10.3) min with neostigmine in Chinese subjects. Overall, 230 Chinese subjects (sugammadex, n = 119, neostigmine, n = 111) and 59 Caucasian subjects (sugammadex, n = 29, neostigmine, n = 30) had evaluable data.
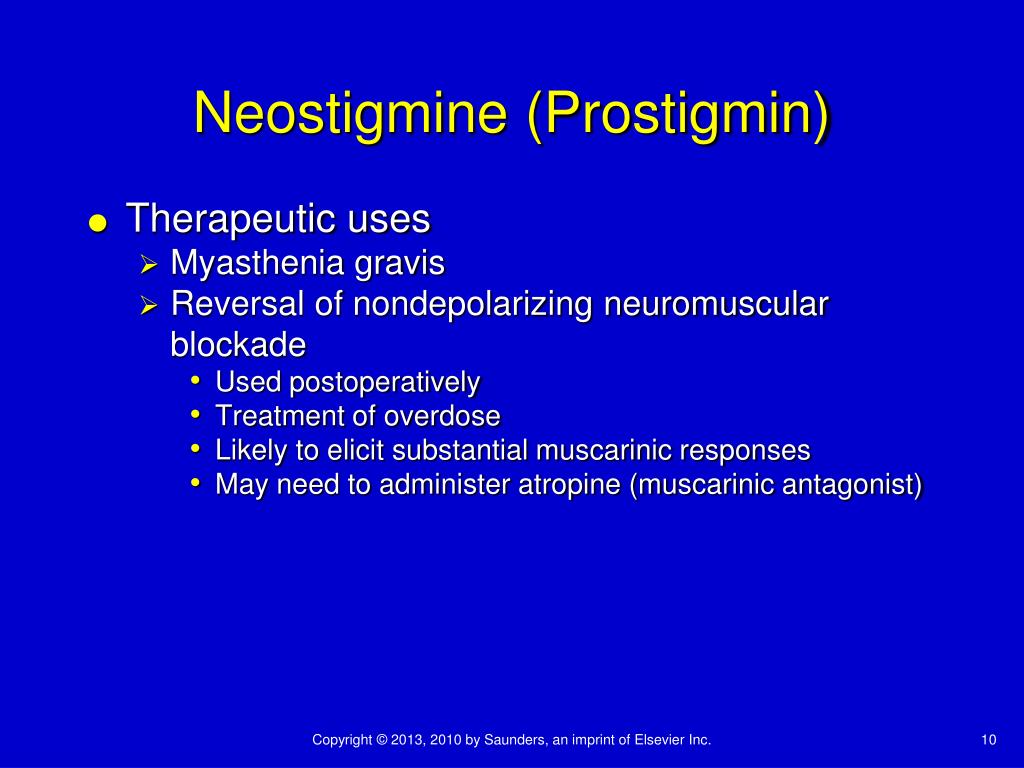
Primary efficacy variable was time from sugammadex/neostigmine to recovery of the train-of-four (TOF) ratio to 0.9. At second twitch reappearance, after last rocuronium dose, subjects received sugammadex 2 mg/kg or neostigmine 50 μg/kg plus atropine 10–20 μg/kg, according to randomization. Rocuronium 0.6 mg/kg was administered for endotracheal intubation, with 0.1–0.2 mg/kg maintenance doses given as required. This was a randomized, active-controlled, multicenter, safety-assessor-blinded study (NCT00825812) in American Society of Anesthesiologists Class 1-3 subjects undergoing surgery with propofol anesthesia. This study compared efficacy and safety of the selective relaxant binding agent sugammadex (2 mg/kg) with neostigmine (50 μg/kg) for neuromuscular blockade (NMB) reversal in Chinese and Caucasian subjects.


 0 kommentar(er)
0 kommentar(er)
